In today's rapidly evolving healthcare landscape, the demand for proficient medical coders is on the rise. These skilled professionals serve as the backbone of the healthcare revenue cycle, translating complex medical procedures and diagnoses into standardized codes used for billing and insurance purposes. As such, obtaining a certification in medical coding has become increasingly important for those looking to advance their careers in this vital sector. Among the most recognized certifications is the one offered by the American Academy of Professional Coders (AAPC), which sets a benchmark for excellence in the field.
The journey toward AAPC certification requires meticulous preparation and a deep understanding of medical coding principles. This rigorous process ensures that candidates are well-equipped to handle real-world challenges in their professional roles. Certification not only signifies a coder's competence but also demonstrates their commitment to maintaining high standards of accuracy and integrity, which are crucial in ensuring proper reimbursement and compliance with healthcare regulations.
Preparing for the AAPC Certification Exam involves a comprehensive review of various components within medical coding. Candidates must familiarize themselves with different code sets, including ICD-10-CM for diagnoses, CPT for procedures, and HCPCS Level II for supplies and services. Additionally, they need to grasp anatomy and physiology concepts to accurately interpret clinical documentation. The exam tests not just rote memorization but also critical thinking skills required to navigate complex scenarios that coders encounter daily.
Beyond technical knowledge, successful candidates often cultivate excellent time-management skills during their preparation. The exam is timed, demanding both speed and precision from examinees who must swiftly tackle multiple-choice questions under pressure. Therefore, adopting effective study strategies-such as taking practice exams or participating in study groups-can significantly enhance one's ability to perform well on test day.
Achieving AAPC certification offers numerous benefits beyond personal satisfaction. For employers, certified coders signify reliability; they are more likely to deliver accurate work promptly while minimizing errors that could lead to denied claims or audits. Consequently, certified professionals often enjoy better job prospects as employers prioritize them over non-certified individuals when hiring.
Moreover, certification can open doors to career advancement opportunities within healthcare organizations or even pave the way towards specialized areas like auditing or education-a testament to its value as an investment into one's future.
In conclusion, understanding the importance of medical coding certification is essential when preparing for the AAPC Certification Exam. It represents not just an individual's mastery over technical skills but also reflects dedication towards upholding quality standards within healthcare systems worldwide-a role indispensable amidst ever-growing demands on this crucial sector's workforce today.
Preparing for the AAPC Certification Exam requires a clear understanding of the various certifications offered by the American Academy of Professional Coders (AAPC) and their respective requirements. AAPC certifications are recognized benchmarks in the healthcare industry, signifying proficiency in medical coding, billing, auditing, compliance, and practice management. Each certification caters to different roles within the healthcare system and has specific prerequisites that candidates must meet.
One of the most popular AAPC certifications is the Certified Professional Coder (CPC) credential. This certification demonstrates mastery over medical coding guidelines and practices across various settings such as physician offices and outpatient facilities. To qualify for the CPC exam, candidates should ideally have at least two years of professional experience or complete an approved medical coding course. The exam tests knowledge in areas like anatomy, medical terminology, and coding guidelines using CPT®, ICD-10-CM, and HCPCS Level II codes.
For those focusing on inpatient hospital coding, the Certified Inpatient Coder (CIC) is more appropriate. The CIC credential is designed for individuals who wish to specialize in inpatient hospital coding with a deep understanding of ICD-10-CM/PCS code sets used in hospitals. Similar to CPC requirements, having relevant work experience or educational coursework significantly enhances one's preparation for this challenging exam.
Another notable certification is the Certified Outpatient Coder (COC), which caters to coders working in outpatient hospital settings. It encompasses skills necessary for accurate ambulatory surgical center coding and outpatient hospital services. Candidates are expected to be familiar with payment methodologies like OPPS and APCs alongside traditional code sets.
For professionals aiming at leadership roles or interested in compliance auditing within healthcare institutions, obtaining a Certified Professional Medical Auditor (CPMA) certification can be advantageous. This credential focuses on skills needed to ensure healthcare providers comply with regulatory standards through effective auditing techniques. Prior experience or training in medical auditing principles can provide a solid foundation for tackling this exam.
The Certified Professional Biller (CPB) certification addresses another facet of healthcare administration by validating expertise in managing revenue cycles through efficient billing practices. Candidates looking into CPB should understand payer requirements, claim submissions processes, and denial management strategies.
Lastly, those aspiring towards managerial positions might consider pursuing the Certified Physician Practice Manager (CPPM) credential. It validates competencies required to effectively manage physician practices encompassing financial management, HR issues, compliance regulations among others often necessitating prior managerial experience or education related to practice management.
In preparing for any AAPC certification exam it's crucial not only to study relevant materials thoroughly but also engage actively with practice exams offered by AAPC resources; these simulate real testing scenarios helping bridge knowledge gaps while building confidence under timed conditions typical during actual examinations.
Overall each AAPC certification opens distinct career pathways within healthcare yet shares commonalities: they demand dedication towards continual learning given ever-evolving industry regulations impacting how care delivery systems operate efficiently today ensuring practitioners remain indispensable assets amidst dynamic landscapes shaping future trajectories forward across disciplines alike globally thereby enhancing professional credibility significantly throughout diverse health sector ecosystems worldwide!
Preparing for the AAPC Certification Exam is a significant undertaking that demands a strategic approach and access to appropriate study materials and resources. Achieving certification from the American Academy of Professional Coders (AAPC) is a milestone in the career of any medical coder, signaling proficiency and dedication to maintaining high industry standards. To ensure success, candidates must equip themselves with a comprehensive toolkit of study aids designed to cover all aspects of the exam content.
First and foremost, obtaining the official AAPC study guides is essential. These guides are meticulously crafted by experts who understand both the breadth and depth of knowledge required to pass the exam. They provide detailed explanations of coding guidelines, healthcare regulations, and medical terminology, ensuring a solid foundational understanding. Additionally, these guides often include practice questions that mirror those found on the actual exam, allowing candidates to familiarize themselves with question formats and time constraints.
Beyond official guides, engaging with online courses can provide an interactive learning experience that caters to diverse learning styles. Many reputable platforms offer video tutorials led by seasoned instructors who break down complex topics into digestible segments. This format not only enhances comprehension but also allows for flexible scheduling-an important consideration for busy professionals balancing work and study.
Participating in study groups or forums can also be invaluable. These communities offer support by connecting individuals embarking on similar journeys. Engaging in discussions about challenging topics or sharing tips on effective study techniques can enhance understanding while providing motivation through shared goals. Platforms like Facebook groups or dedicated forums such as AAPC's own member community facilitate these interactions.
Practice exams are another crucial component in preparing for the AAPC certification exam. These tests simulate real exam conditions, helping students develop strategies for managing time effectively and reducing test anxiety. Repeatedly working through practice exams enables individuals to identify areas where they may need further review while reinforcing strengths.
In addition to structured materials, personal organization plays a pivotal role in successful exam preparation. Creating a realistic study plan that outlines daily or weekly goals helps maintain steady progress towards readiness without feeling overwhelmed. Allocating specific times for different content areas ensures balanced coverage across all subjects tested in the exam.
Lastly, leveraging mobile apps focused on medical coding can turn spare moments into productive learning opportunities. Apps offering flashcards or quick quizzes allow candidates to reinforce their knowledge during commutes or breaks from routine tasks.
In conclusion, preparing for the AAPC Certification Exam requires more than just rote memorization; it demands engagement with a variety of high-quality resources tailored to individual learning preferences and schedules. By integrating official study materials with interactive courses, community interaction, practice exams, personal organization strategies, and technological tools such as mobile apps, aspiring certified professional coders can approach their exam with confidence rooted in thorough preparation-a critical step towards advancing their careers within this vital sector of healthcare administration.
Preparing for the AAPC Certification Exam can be a daunting task, but with effective study strategies and time management tips, you can enhance your chances of success. Achieving certification not only demonstrates your expertise in medical coding but also opens doors to numerous career opportunities. To tackle this challenge efficiently, it's essential to employ a structured approach that accommodates both content mastery and personal well-being.
First and foremost, understanding the exam format is crucial. The AAPC Certification Exam tests your knowledge on various aspects of medical coding, including anatomy, physiology, medical terminology, and coding guidelines. Familiarize yourself with the exam structure and content by reviewing official materials provided by AAPC. This will help you identify key areas where you need more focus.
One effective study strategy is to create a comprehensive study plan. Break down the syllabus into manageable segments and allocate specific time slots for each topic. Establishing a routine helps maintain consistency and reduces last-minute cramming sessions that often lead to burnout. Utilize active learning techniques such as flashcards for memorization or practice exams to simulate the test environment and assess your progress.
Moreover, leveraging available resources can significantly boost your preparation efforts. Consider joining study groups or online forums where you can engage with fellow candidates. Sharing insights and discussing challenging topics fosters a collaborative learning environment that can clarify doubts and reinforce understanding.
Time management plays an integral role in balancing life commitments with exam preparation. Prioritize tasks by setting realistic goals daily or weekly, ensuring that they align with the overall timeline leading up to the exam date. Incorporate regular breaks into your schedule to prevent fatigue; short intervals of rest have been proven to enhance concentration levels when returning to study.
Additionally, maintaining a healthy lifestyle contributes positively to cognitive performance during preparation. Ensure adequate sleep, nutritious meals, and physical activity are part of your daily regimen-these elements improve mental alertness and reduce stress levels.
In conclusion, preparing for the AAPC Certification Exam demands dedication, strategic planning, and efficient time management. By understanding the exam format thoroughly, creating structured study plans, engaging in active learning methods, utilizing community resources effectively, managing time wisely while prioritizing self-care-you set yourself up for success not only on exam day but also in your future endeavors within the medical coding profession.
Preparing for the AAPC Certification Exam is a crucial step for those aiming to excel in the field of medical coding. The American Academy of Professional Coders (AAPC) certification is highly regarded and can significantly enhance one's career prospects. However, achieving this certification requires diligence, dedication, and strategic preparation. One effective method to ensure readiness is through practice exams and sample questions, which serve as invaluable tools for familiarization with the exam format and content.
Practice exams mimic the structure of the actual AAPC exam, allowing candidates to experience firsthand what they will encounter on test day. This familiarity helps reduce anxiety and builds confidence, as test-takers become comfortable with the types of questions they will face. By simulating real exam conditions, individuals can gauge their time management skills and identify areas where they need improvement. This iterative process of practice and review ensures that candidates are not only knowledgeable but also efficient in applying their knowledge under time constraints.
Sample questions provide a focused means of understanding specific concepts within medical coding. These questions often highlight key topics that are frequently tested, offering insights into important areas that require mastery. Working through these samples enables candidates to deepen their understanding of complex codes, guidelines, and scenarios they might encounter during the exam. Moreover, analyzing incorrect responses allows learners to pinpoint weaknesses in their grasp of certain subjects or coding principles.
In addition to boosting technical proficiency, practice exams and sample questions cultivate critical thinking skills essential for success on the AAPC Certification Exam. Medical coding is not just about memorizing codes; it involves interpreting patient information accurately and translating it into standardized codes with precision. Through regular practice with varied question formats-such as multiple-choice or case studies-candidates sharpen their analytical abilities and improve their decision-making processes.
Furthermore, engaging with practice materials fosters a disciplined study routine necessary for effective preparation. It encourages consistent effort over cramming sessions at the last minute. Establishing a study schedule that incorporates regular practice exams creates a structured path towards gradual improvement and sustained learning.
In conclusion, utilizing practice exams and sample questions is an indispensable strategy in preparing for the AAPC Certification Exam. These resources offer candidates an opportunity to familiarize themselves with exam conditions while honing both technical knowledge and critical thinking skills. With diligent use of these tools alongside comprehensive study materials, aspiring certified medical coders can approach their examination journey well-prepared and confident in achieving certification success.
Preparing for the AAPC Certification Exam is a significant milestone for aspiring medical coders, and with it comes the inevitable stress of test day. However, effective preparation and stress management can transform this daunting experience into an opportunity to showcase your hard-earned knowledge and skills.
The first step in preparing for the AAPC exam is to establish a structured study plan well in advance of the test date. This plan should encompass a comprehensive review of all necessary materials, including textbooks, coding manuals, and practice exams. Consistency is key; dedicating regular study sessions each week will help reinforce your understanding over time. Utilizing various resources such as online courses or study groups can also provide diverse perspectives on challenging topics.
Another crucial aspect of preparation is familiarizing yourself with the exam format. Understanding how questions are structured and timed will enable you to approach the exam with confidence. Practice exams are invaluable here-they not only highlight areas needing improvement but also acclimate you to the pace required during the actual test.
As test day approaches, mental readiness becomes just as important as academic preparation. Stress management techniques are essential in ensuring that anxiety does not hinder performance. Begin by maintaining a healthy lifestyle: adequate sleep, balanced nutrition, and regular exercise are fundamental in keeping both body and mind sharp.
Mindfulness practices such as meditation or deep-breathing exercises can significantly reduce stress levels. Taking a few minutes each day to clear your mind can enhance focus and calmness-qualities beneficial on exam day. Additionally, visualization techniques can be powerful; imagine yourself confidently navigating through the exam, which can boost self-assurance when under pressure.
On the morning of the exam, start with a nutritious breakfast that includes proteins and complex carbohydrates to sustain energy levels throughout the test duration. Arrive at the testing center early to avoid last-minute rush-induced stressors.
During the exam itself, manage your time wisely-allocate specific periods for each section based on its complexity and length. If you encounter difficult questions, remain calm; mark them for review if possible and move on-returning later with a fresh perspective might reveal solutions more easily.
Lastly, maintain positive self-talk throughout your preparations and during the test itself. Remind yourself of your dedication and preparedness-this positivity fosters resilience against any setbacks encountered during testing.
In summary, preparing for the AAPC Certification Exam involves both thorough academic preparation and strategic stress management techniques. By balancing these elements effectively, candidates can approach their certification journey with confidence-poised not only to succeed but to excel in their professional aspirations within medical coding fields.
| Part of a series on |
| Accounting |
|---|
 |
|
Financial statement analysis (or just financial analysis) is the process of reviewing and analyzing a company's financial statements to make better economic decisions to earn income in future. These statements include the income statement, balance sheet, statement of cash flows, notes to accounts and a statement of changes in equity (if applicable). Financial statement analysis is a method or process involving specific techniques for evaluating risks, performance, valuation, financial health, and future prospects of an organization.[1]
It is used by a variety of stakeholders, such as credit and equity investors, the government, the public, and decision-makers within the organization. These stakeholders have different interests and apply a variety of different techniques to meet their needs. For example, equity investors are interested in the long-term earnings power of the organization and perhaps the sustainability and growth of dividend payments. Creditors want to ensure the interest and principal is paid on the organizations debt securities (e.g., bonds) when due.
Common methods of financial statement analysis include horizontal and vertical analysis and the use of financial ratios. Historical information combined with a series of assumptions and adjustments to the financial information may be used to project future performance. The Chartered Financial Analyst designation is available for professional financial analysts.
Benjamin Graham and David Dodd first published their influential book "Security Analysis" in 1934.[2] [3] A central premise of their book is that the market's pricing mechanism for financial securities such as stocks and bonds is based upon faulty and irrational analytical processes performed by many market participants. This results in the market price of a security only occasionally coinciding with the intrinsic value around which the price tends to fluctuate.[4] Investor Warren Buffett is a well-known supporter of Graham and Dodd's philosophy.
The Graham and Dodd approach is referred to as Fundamental analysis and includes: 1) Economic analysis; 2) Industry analysis; and 3) Company analysis. The latter is the primary realm of financial statement analysis. On the basis of these three analyses the intrinsic value of the security is determined.[4]
Horizontal analysis compares financial information over time, typically from past quarters or years. Horizontal analysis is performed by comparing financial data from a past statement, such as the income statement. When comparing this past information one will want to look for variations such as higher or lower earnings.[5]
Vertical analysis is a percentage analysis of financial statements. Each line item listed in the financial statement is listed as the percentage of another line item. For example, on an income statement each line item will be listed as a percentage of gross sales. This technique is also referred to as normalization[6] or common-sizing.[5]
Financial ratios are very powerful tools to perform some quick analysis of financial statements. There are four main categories of ratios: liquidity ratios, profitability ratios, activity ratios and leverage ratios. These are typically analyzed over time and across competitors in an industry.
DuPont analysis uses several financial ratios that multiplied together equal return on equity, a measure of how much income the firm earns divided by the amount of funds invested (equity).
A Dividend discount model (DDM) may also be used to value a company's stock price based on the theory that its stock is worth the sum of all of its future dividend payments, discounted back to their present value.[8] In other words, it is used to value stocks based on the net present value of the future dividends.
Financial statement analyses are typically performed in spreadsheet software — or specialized accounting software — and summarized in a variety of formats.
An earnings recast is the act of amending and re-releasing a previously released earnings statement, with specified intent.[9]
Investors need to understand the ability of the company to generate profit. This, together with its rate of profit growth, relative to the amount of capital deployed and various other financial ratios, forms an important part of their analysis of the value of the company. Analysts may modify ("recast") the financial statements by adjusting the underlying assumptions to aid in this computation. For example, operating leases (treated like a rental transaction) may be recast as capital leases (indicating ownership), adding assets and liabilities to the balance sheet. This affects the financial statement ratios.[10]
Recasting is also known as normalizing accounts.[11]
Financial analysts typically have finance and accounting education at the undergraduate or graduate level. Persons may earn the Chartered Financial Analyst (CFA) designation through a series of challenging examinations. Upon completion of the three-part exam, CFAs are considered experts in areas like fundamentals of investing, the valuation of assets, portfolio management, and wealth planning.
Health has a variety of definitions, which have been used for different purposes over time. In general, it refers to physical and emotional well-being, especially that associated with normal functioning of the human body, absent of disease, pain (including mental pain), or injury.
Health can be promoted by encouraging healthful activities, such as regular physical exercise and adequate sleep,[1] and by reducing or avoiding unhealthful activities or situations, such as smoking or excessive stress. Some factors affecting health are due to individual choices, such as whether to engage in a high-risk behavior, while others are due to structural causes, such as whether the society is arranged in a way that makes it easier or harder for people to get necessary healthcare services. Still, other factors are beyond both individual and group choices, such as genetic disorders.
Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.
The meaning of health has evolved over time. In keeping with the biomedical perspective, early definitions of health focused on the theme of the body's ability to function; health was seen as a state of normal function that could be disrupted from time to time by disease. An example of such a definition of health is: "a state characterized by anatomic, physiologic, and psychological integrity; ability to perform personally valued family, work, and community roles; ability to deal with physical, biological, psychological, and social stress".[2] Then, in 1948, in a radical departure from previous definitions, the World Health Organization (WHO) proposed a definition that aimed higher, linking health to well-being, in terms of "physical, mental, and social well-being, and not merely the absence of disease and infirmity".[3] Although this definition was welcomed by some as being innovative, it was also criticized for being vague and excessively broad and was not construed as measurable. For a long time, it was set aside as an impractical ideal, with most discussions of health returning to the practicality of the biomedical model.[4]
Just as there was a shift from viewing disease as a state to thinking of it as a process, the same shift happened in definitions of health. Again, the WHO played a leading role when it fostered the development of the health promotion movement in the 1980s. This brought in a new conception of health, not as a state, but in dynamic terms of resiliency, in other words, as "a resource for living". In 1984, WHO revised the definition of health defined it as "the extent to which an individual or group is able to realize aspirations and satisfy needs and to change or cope with the environment. Health is a resource for everyday life, not the objective of living; it is a positive concept, emphasizing social and personal resources, as well as physical capacities."[5] Thus, health referred to the ability to maintain homeostasis and recover from adverse events. Mental, intellectual, emotional and social health referred to a person's ability to handle stress, to acquire skills, to maintain relationships, all of which form resources for resiliency and independent living.[4] This opens up many possibilities for health to be taught, strengthened and learned.
Since the late 1970s, the federal Healthy People Program has been a visible component of the United States' approach to improving population health.[6] In each decade, a new version of Healthy People is issued,[7] featuring updated goals and identifying topic areas and quantifiable objectives for health improvement during the succeeding ten years, with assessment at that point of progress or lack thereof. Progress has been limited to many objectives, leading to concerns about the effectiveness of Healthy People in shaping outcomes in the context of a decentralized and uncoordinated US health system. Healthy People 2020 gives more prominence to health promotion and preventive approaches and adds a substantive focus on the importance of addressing social determinants of health. A new expanded digital interface facilitates use and dissemination rather than bulky printed books as produced in the past. The impact of these changes to Healthy People will be determined in the coming years.[8]
Systematic activities to prevent or cure health problems and promote good health in humans are undertaken by health care providers. Applications with regard to animal health are covered by the veterinary sciences. The term "healthy" is also widely used in the context of many types of non-living organizations and their impacts for the benefit of humans, such as in the sense of healthy communities, healthy cities or healthy environments. In addition to health care interventions and a person's surroundings, a number of other factors are known to influence the health status of individuals. These are referred to as the "determinants of health", which include the individual's background, lifestyle, economic status, social conditions and spirituality; Studies have shown that high levels of stress can affect human health.[9]
In the first decade of the 21st century, the conceptualization of health as an ability opened the door for self-assessments to become the main indicators to judge the performance of efforts aimed at improving human health.[10] It also created the opportunity for every person to feel healthy, even in the presence of multiple chronic diseases or a terminal condition, and for the re-examination of determinants of health (away from the traditional approach that focuses on the reduction of the prevalence of diseases).[11]
In general, the context in which an individual lives is of great importance for both his health status and quality of life. It is increasingly recognized that health is maintained and improved not only through the advancement and application of health science, but also through the efforts and intelligent lifestyle choices of the individual and society. According to the World Health Organization, the main determinants of health include the social and economic environment, the physical environment, and the person's individual characteristics and behaviors.[12]
More specifically, key factors that have been found to influence whether people are healthy or unhealthy include the following:[12][13][14]
|
|

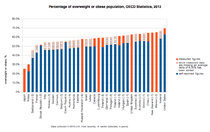
An increasing number of studies and reports from different organizations and contexts examine the linkages between health and different factors, including lifestyles, environments, health care organization and health policy, one specific health policy brought into many countries in recent years was the introduction of the sugar tax. Beverage taxes came into light with increasing concerns about obesity, particularly among youth. Sugar-sweetened beverages have become a target of anti-obesity initiatives with increasing evidence of their link to obesity.[15]—such as the 1974 Lalonde report from Canada;[14] the Alameda County Study in California;[16] and the series of World Health Reports of the World Health Organization, which focuses on global health issues including access to health care and improving public health outcomes, especially in developing countries.[17]
The concept of the "health field," as distinct from medical care, emerged from the Lalonde report from Canada. The report identified three interdependent fields as key determinants of an individual's health. These are:[14]
The maintenance and promotion of health is achieved through different combination of physical, mental, and social well-being—a combination sometimes referred to as the "health triangle."[18] The WHO's 1986 Ottawa Charter for Health Promotion further stated that health is not just a state, but also "a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities."[19]
Focusing more on lifestyle issues and their relationships with functional health, data from the Alameda County Study suggested that people can improve their health via exercise, enough sleep, spending time in nature, maintaining a healthy body weight, limiting alcohol use, and avoiding smoking.[20] Health and illness can co-exist, as even people with multiple chronic diseases or terminal illnesses can consider themselves healthy.[21]
If you want to learn about the health of a population, look at the air they breathe, the water they drink, and the places where they live.[22][23]
— Hippocrates, the Father of Medicine, 5th century BC
The environment is often cited as an important factor influencing the health status of individuals. This includes characteristics of the natural environment, the built environment and the social environment. Factors such as clean water and air, adequate housing, and safe communities and roads all have been found to contribute to good health, especially to the health of infants and children.[12][24] Some studies have shown that a lack of neighborhood recreational spaces including natural environment leads to lower levels of personal satisfaction and higher levels of obesity, linked to lower overall health and well-being.[25] It has been demonstrated that increased time spent in natural environments is associated with improved self-reported health,[26] suggesting that the positive health benefits of natural space in urban neighborhoods should be taken into account in public policy and land use.
Genetics, or inherited traits from parents, also play a role in determining the health status of individuals and populations. This can encompass both the predisposition to certain diseases and health conditions, as well as the habits and behaviors individuals develop through the lifestyle of their families. For example, genetics may play a role in the manner in which people cope with stress, either mental, emotional or physical. For example, obesity is a significant problem in the United States that contributes to poor mental health and causes stress in the lives of many people.[27] One difficulty is the issue raised by the debate over the relative strengths of genetics and other factors; interactions between genetics and environment may be of particular importance.
A number of health issues are common around the globe. Disease is one of the most common. According to GlobalIssues.org, approximately 36 million people die each year from non-communicable (i.e., not contagious) diseases, including cardiovascular disease, cancer, diabetes and chronic lung disease.[28]
Among communicable diseases, both viral and bacterial, AIDS/HIV, tuberculosis, and malaria are the most common, causing millions of deaths every year.[28]
Another health issue that causes death or contributes to other health problems is malnutrition, especially among children. One of the groups malnutrition affects most is young children. Approximately 7.5 million children under the age of 5 die from malnutrition, usually brought on by not having the money to find or make food.[28]
Bodily injuries are also a common health issue worldwide. These injuries, including bone fractures and burns, can reduce a person's quality of life or can cause fatalities including infections that resulted from the injury (or the severity injury in general).[28]
Lifestyle choices are contributing factors to poor health in many cases. These include smoking cigarettes, and can also include a poor diet, whether it is overeating or an overly constrictive diet. Inactivity can also contribute to health issues and also a lack of sleep, excessive alcohol consumption, and neglect of oral hygiene.[citation needed] There are also genetic disorders that are inherited by the person and can vary in how much they affect the person (and when they surface).[29][30]
Although the majority of these health issues are preventable, a major contributor to global ill health is the fact that approximately 1 billion people lack access to health care systems.[28] Arguably, the most common and harmful health issue is that a great many people do not have access to quality remedies.[31]
The World Health Organization describes mental health as "a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community".[32] Mental health is not just the absence of mental illness.[33]
Mental illness is described as 'the spectrum of cognitive, emotional, and behavioral conditions that interfere with social and emotional well-being and the lives and productivity of people.[34] Having a mental illness can seriously impair, temporarily or permanently, the mental functioning of a person. Other terms include: 'mental health problem', 'illness', 'disorder', 'dysfunction'.[35]
Approximately twenty percent of all adults in the US are considered diagnosable with a mental disorder. Mental disorders are the leading cause of disability in the United States and Canada. Examples of these disorders include schizophrenia, ADHD, major depressive disorder, bipolar disorder, anxiety disorder, post-traumatic stress disorder and autism.[36]
Many factors contribute to mental health problems, including:[37]
Achieving and maintaining health is an ongoing process, shaped by both the evolution of health care knowledge and practices as well as personal strategies and organized interventions for staying healthy.
An important way to maintain one's personal health is to have a healthy diet. A healthy diet includes a variety of plant-based and animal-based foods that provide nutrients to the body.[41] Such nutrients provide the body with energy and keep it running. Nutrients help build and strengthen bones, muscles, and tendons and also regulate body processes (i.e., blood pressure). Water is essential for growth, reproduction and good health. Macronutrients are consumed in relatively large quantities and include proteins, carbohydrates, and fats and fatty acids.[42] Micronutrients – vitamins and minerals – are consumed in relatively smaller quantities, but are essential to body processes.[43] The food guide pyramid is a pyramid-shaped guide of healthy foods divided into sections. Each section shows the recommended intake for each food group (i.e., protein, fat, carbohydrates and sugars). Making healthy food choices can lower one's risk of heart disease and the risk of developing some types of cancer, and can help one maintain their weight within a healthy range.[44]
The Mediterranean diet is commonly associated with health-promoting effects. This is sometimes attributed to the inclusion of bioactive compounds such as phenolic compounds, isoprenoids and alkaloids.[45]
Physical exercise enhances or maintains physical fitness and overall health and wellness. It strengthens one's bones and muscles and improves the cardiovascular system. According to the National Institutes of Health, there are four types of exercise: endurance, strength, flexibility, and balance.[46] The CDC states that physical exercise can reduce the risks of heart disease, cancer, type 2 diabetes, high blood pressure, obesity, depression, and anxiety.[47] For the purpose of counteracting possible risks, it is often recommended to start physical exercise gradually as one goes. Participating in any exercising, whether it is housework, yardwork, walking or standing up when talking on the phone, is often thought to be better than none when it comes to health.[48]
Sleep is an essential component to maintaining health. In children, sleep is also vital for growth and development. Ongoing sleep deprivation has been linked to an increased risk for some chronic health problems. In addition, sleep deprivation has been shown to correlate with both increased susceptibility to illness and slower recovery times from illness.[49] In one study, people with chronic insufficient sleep, set as six hours of sleep a night or less, were found to be four times more likely to catch a cold compared to those who reported sleeping for seven hours or more a night.[50] Due to the role of sleep in regulating metabolism, insufficient sleep may also play a role in weight gain or, conversely, in impeding weight loss.[51] Additionally, in 2007, the International Agency for Research on Cancer, which is the cancer research agency for the World Health Organization, declared that "shiftwork that involves circadian disruption is probably carcinogenic to humans", speaking to the dangers of long-term nighttime work due to its intrusion on sleep.[52] In 2015, the National Sleep Foundation released updated recommendations for sleep duration requirements based on age, and concluded that "Individuals who habitually sleep outside the normal range may be exhibiting signs or symptoms of serious health problems or, if done volitionally, may be compromising their health and well-being."[53]
| Age and condition | Sleep needs |
|---|---|
| Newborns (0–3 months) | 14 to 17 hours |
| Infants (4–11 months) | 12 to 15 hours |
| Toddlers (1–2 years) | 11 to 14 hours |
| Preschoolers (3–5 years) | 10 to 13 hours |
| School-age children (6–13 years) | 9 to 11 hours |
| Teenagers (14–17 years) | 8 to 10 hours |
| Adults (18–64 years) | 7 to 9 hours |
| Older Adults (65 years and over) | 7 to 8 hours |
Health science is the branch of science focused on health. There are two main approaches to health science: the study and research of the body and health-related issues to understand how humans (and animals) function, and the application of that knowledge to improve health and to prevent and cure diseases and other physical and mental impairments. The science builds on many sub-fields, including biology, biochemistry, physics, epidemiology, pharmacology, medical sociology. Applied health sciences endeavor to better understand and improve human health through applications in areas such as health education, biomedical engineering, biotechnology and public health.[citation needed]
Organized interventions to improve health based on the principles and procedures developed through the health sciences are provided by practitioners trained in medicine, nursing, nutrition, pharmacy, social work, psychology, occupational therapy, physical therapy and other health care professions. Clinical practitioners focus mainly on the health of individuals, while public health practitioners consider the overall health of communities and populations. Workplace wellness programs are increasingly being adopted by companies for their value in improving the health and well-being of their employees, as are school health services to improve the health and well-being of children.[citation needed]
Contemporary medicine is in general conducted within health care systems. Legal, credentialing and financing frameworks are established by individual governments, augmented on occasion by international organizations, such as churches. The characteristics of any given health care system have significant impact on the way medical care is provided.
From ancient times, Christian emphasis on practical charity gave rise to the development of systematic nursing and hospitals and the Catholic Church today remains the largest non-government provider of medical services in the world.[54] Advanced industrial countries (with the exception of the United States)[55] and many developing countries provide medical services through a system of universal health care that aims to guarantee care for all through a single-payer health care system, or compulsory private or co-operative health insurance. This is intended to ensure that the entire population has access to medical care on the basis of need rather than ability to pay. Delivery may be via private medical practices or by state-owned hospitals and clinics, or by charities, most commonly by a combination of all three.
Most tribal societies provide no guarantee of healthcare for the population as a whole.[56] In such societies, healthcare is available to those that can afford to pay for it or have self-insured it (either directly or as part of an employment contract) or who may be covered by care financed by the government or tribe directly.

Transparency of information is another factor defining a delivery system. Access to information on conditions, treatments, quality, and pricing greatly affects the choice by patients/consumers and, therefore, the incentives of medical professionals. While the US healthcare system has come under fire for lack of openness,[57] new legislation may encourage greater openness. There is a perceived tension between the need for transparency on the one hand and such issues as patient confidentiality and the possible exploitation of information for commercial gain on the other.
Provision of medical care is classified into primary, secondary, and tertiary care categories.[58]

Primary care medical services are provided by physicians, physician assistants, nurse practitioners, or other health professionals who have first contact with a patient seeking medical treatment or care.[59] These occur in physician offices, clinics, nursing homes, schools, home visits, and other places close to patients. About 90% of medical visits can be treated by the primary care provider. These include treatment of acute and chronic illnesses, preventive care and health education for all ages and both sexes.
Secondary care medical services are provided by medical specialists in their offices or clinics or at local community hospitals for a patient referred by a primary care provider who first diagnosed or treated the patient.[60] Referrals are made for those patients who required the expertise or procedures performed by specialists. These include both ambulatory care and inpatient services, Emergency departments, intensive care medicine, surgery services, physical therapy, labor and delivery, endoscopy units, diagnostic laboratory and medical imaging services, hospice centers, etc. Some primary care providers may also take care of hospitalized patients and deliver babies in a secondary care setting.
Tertiary care medical services are provided by specialist hospitals or regional centers equipped with diagnostic and treatment facilities not generally available at local hospitals. These include trauma centers, burn treatment centers, advanced neonatology unit services, organ transplants, high-risk pregnancy, radiation oncology, etc.
Modern medical care also depends on information – still delivered in many health care settings on paper records, but increasingly nowadays by electronic means.
In low-income countries, modern healthcare is often too expensive for the average person. International healthcare policy researchers have advocated that "user fees" be removed in these areas to ensure access, although even after removal, significant costs and barriers remain.[61]
Separation of prescribing and dispensing is a practice in medicine and pharmacy in which the physician who provides a medical prescription is independent from the pharmacist who provides the prescription drug. In the Western world there are centuries of tradition for separating pharmacists from physicians. In Asian countries, it is traditional for physicians to also provide drugs.[62]
Public health has been described as "the science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals."[63] It is concerned with threats to the overall health of a community based on population health analysis. The population in question can be as small as a handful of people or as large as all the inhabitants of several continents (for instance, in the case of a pandemic). Public health has many sub-fields, but typically includes the interdisciplinary categories of epidemiology, biostatistics and health services. environmental health, community health, behavioral health, and occupational health are also important areas of public health.
The focus of public health interventions is to prevent and manage diseases, injuries and other health conditions through surveillance of cases and the promotion of healthy behavior, communities, and (in aspects relevant to human health) environments. Its aim is to prevent health problems from happening or re-occurring by implementing educational programs, developing policies, administering services and conducting research.[64] In many cases, treating a disease or controlling a pathogen can be vital to preventing it in others, such as during an outbreak. Vaccination programs and distribution of condoms to prevent the spread of communicable diseases are examples of common preventive public health measures, as are educational campaigns to promote vaccination and the use of condoms (including overcoming resistance to such).
Public health also takes various actions to limit the health disparities between different areas of the country and, in some cases, the continent or world. One issue is the access of individuals and communities to health care in terms of financial, geographical or socio-cultural constraints.[65] Applications of the public health system include the areas of maternal and child health, health services administration, emergency response, and prevention and control of infectious and chronic diseases.
The great positive impact of public health programs is widely acknowledged. Due in part to the policies and actions developed through public health, the 20th century registered a decrease in the mortality rates for infants and children and a continual increase in life expectancy in most parts of the world. For example, it is estimated that life expectancy has increased for Americans by thirty years since 1900,[66] and worldwide by six years since 1990.[67]

Personal health depends partially on the active, passive, and assisted cues people observe and adopt about their own health. These include personal actions for preventing or minimizing the effects of a disease, usually a chronic condition, through integrative care. They also include personal hygiene practices to prevent infection and illness, such as bathing and washing hands with soap; brushing and flossing teeth; storing, preparing and handling food safely; and many others. The information gleaned from personal observations of daily living – such as about sleep patterns, exercise behavior, nutritional intake and environmental features – may be used to inform personal decisions and actions (e.g., "I feel tired in the morning so I am going to try sleeping on a different pillow"), as well as clinical decisions and treatment plans (e.g., a patient who notices his or her shoes are tighter than usual may be having exacerbation of left-sided heart failure, and may require diuretic medication to reduce fluid overload).[68]
Personal health also depends partially on the social structure of a person's life. The maintenance of strong social relationships, volunteering, and other social activities have been linked to positive mental health and also increased longevity. One American study among seniors over age 70, found that frequent volunteering was associated with reduced risk of dying compared with older persons who did not volunteer, regardless of physical health status.[69] Another study from Singapore reported that volunteering retirees had significantly better cognitive performance scores, fewer depressive symptoms, and better mental well-being and life satisfaction than non-volunteering retirees.[70]
Prolonged psychological stress may negatively impact health, and has been cited as a factor in cognitive impairment with aging, depressive illness, and expression of disease.[71] Stress management is the application of methods to either reduce stress or increase tolerance to stress. Relaxation techniques are physical methods used to relieve stress. Psychological methods include cognitive therapy, meditation, and positive thinking, which work by reducing response to stress. Improving relevant skills, such as problem solving and time management skills, reduces uncertainty and builds confidence, which also reduces the reaction to stress-causing situations where those skills are applicable.
In addition to safety risks, many jobs also present risks of disease, illness and other long-term health problems. Among the most common occupational diseases are various forms of pneumoconiosis, including silicosis and coal worker's pneumoconiosis (black lung disease). Asthma is another respiratory illness that many workers are vulnerable to. Workers may also be vulnerable to skin diseases, including eczema, dermatitis, urticaria, sunburn, and skin cancer.[72] Other occupational diseases of concern include carpal tunnel syndrome and lead poisoning.
As the number of service sector jobs has risen in developed countries, more and more jobs have become sedentary, presenting a different array of health problems than those associated with manufacturing and the primary sector. Contemporary problems, such as the growing rate of obesity and issues relating to stress and overwork in many countries, have further complicated the interaction between work and health.
Many governments view occupational health as a social challenge and have formed public organizations to ensure the health and safety of workers. Examples of these include the British Health and Safety Executive and in the United States, the National Institute for Occupational Safety and Health, which conducts research on occupational health and safety, and the Occupational Safety and Health Administration, which handles regulation and policy relating to worker safety and health.[73]
cite journal: CS1 maint: DOI inactive as of December 2024 (link)